RESEARCH ARTICLE
Additive Manufacturing and Dentistry: Designing a Semi-Physiological Articulator
François-Xavier Santolalla, Etienne Debarre, Philippe Hivart*
Article Information
Identifiers and Pagination:
Year: 2018Volume: 6
First Page: 1
Last Page: 9
Publisher Id: TOMDJ-6-1
DOI: 10.2174/1875181401806010001
Article History:
Received Date: 13/10/2017Revision Received Date: 17/01/2018
Acceptance Date: 29/1/2018
Electronic publication date: 19/02/2018
Collection year: 2018
open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: (https://creativecommons.org/licenses/by/4.0/legalcode). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction:
The use of second generation semi-adjustable articulators for the reproduction of the mandibular kinematic often proves to be a technical and time constraint for the dentist. Therefore, its use, however essential within the dental office, is frequently forsaken.
Materials and methods:
The possibility of reproducing complex anatomical forms using rapid prototyping technologies can induce a more attractive and effective use of such a modified articulator.
Results & Conclusion:
Indeed, these replicas substitute for mechanical adjustments and thereby make the metrology on the patient an unnecessary element, both sources of the approximation of the kinematic. The aim of this study is to report on designing and manufacturing a semi-physiological articulator and on its pertinence through the comparison of the mandibular kinematics movement reproducibility on the two types of articulator.
1. INTRODUCTION
Health is a sensitive subject for the populations, especially when it comes to oral health [1]. Dental problems, as a matter of fact, are described as painful, or can even be visible, with multiple consequences [2]. Among these problems, dysfunction and disorders disrupting the mandibular movements and the teeth contacts of upper and lower jaws at rest or during these movements can be discriminated. Their study defines the dentistry discipline called occlusodontia that corresponds to the study of the masticatory system, of the different pathologies that may affect it and of their care.
Parameters called determinants [3] characterize movements and anatomical relations. Our study deals with those defined in the Fig. (1): the condylar slope, the Bennett angle and the immediate lateral movement (if Temporomandibular Joint TMJ disorders) [4]. The Non-Working Lateral Movement (NWLM) regards the opposite side of the working condyle, contrary to the working one (WLM).
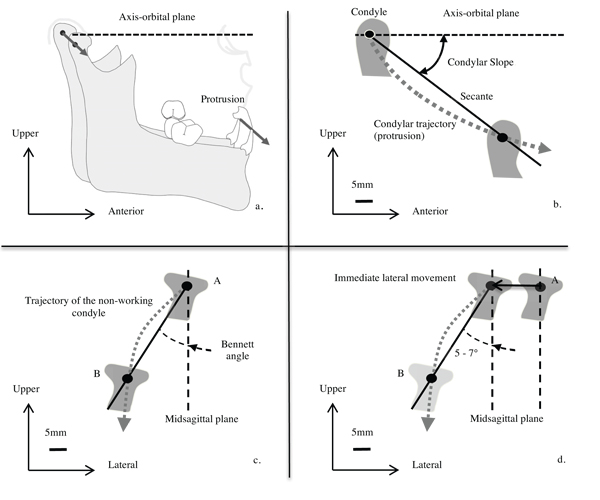 |
Fig. (1). Mandibular kinematic: a. protrusion (sagittal view), b. condylar slope, c. Bennett angle (β), d. immediate lateral movement. |
The opening movement parameter may be added, although it is not determinant. The condyles perform a pure rotation then a translation in the mandibular fossae [5].
The mandibular kinematic is clearly complex. If the metrology on patient is difficult, its study in situ is even more difficult [6, 7]. Investigating the teeth connection requires an articulator or device allowing the repetition of mandibular movements. It helps identifying disorders and pathologies. It can be used as a support of information of a patient and as the basis of the manufacture of a suitable dental prosthesis [8]. It is an indispensable tool in a dental office [9]. It is commonly used, especially in prosthetic rehabilitation context, fixed or removable, unitary or plural or even in diagnosing pathologies of the TMJ.
This simulator allows more or less precise realisation of the mandibular kinematic, according to different adjustments and settings (called programming). Several types are available on the market, according to the complexity of programming. Generally, the more sophisticated it is, the more the realisation of the movements is reliable, but the more its use is difficult and the competence is necessary. Consequently, the standard second generation semi-adjustable articulator is the most used in dental offices, even if it is not the most sophisticated one, but the adjustable one. The reproduction of movements is approximately relative to the physiology of the patient. This approximation is caused by both the difficulty of in situ measurements of the determinants as well as by the mechanical design of the articulators.
We aim to free from the metrology on the patient and its limits of the mechanical adjustments. Therefore, a semi-physiological articulator is obtained by substituting the devices of adjustments and settings of a standard articulator for the replica of the TMJ, which is manufactured by fused deposition modelling from the data of the medical imaging.
Interests of the use of anatomical parts are demonstrated by comparing movements carried out by the standard or modified articulators. Finally, a comparative study based on the axiography of movements of patients and of the modified articulator allows checking the reproducibility of the different movements of the mandibular kinematic.
2. MATERIALS AND METHODS
2.1. Standard Articulator
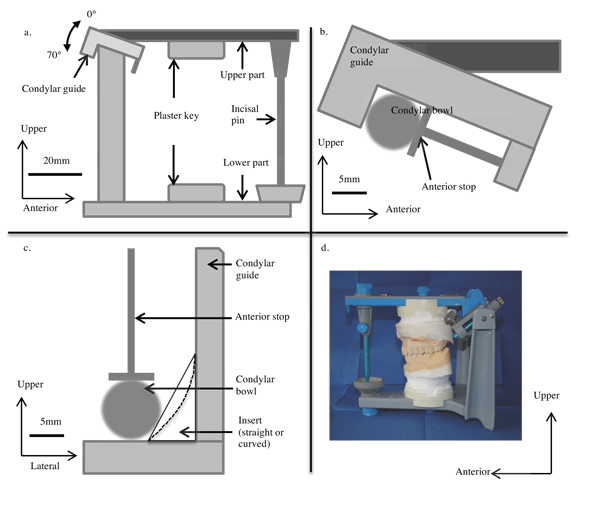
We use a second generation semi-adjustable articulator, semi-adjustable because of its ability to adjust several determinants (the condylar slope, the immediate mandibular lateral movement and the Bennett angle); as a consequence, it is not a fully adjustable one or a non-adjustable one (occludator).
The two parts (upper and lower) that compose it are movable to one another, and allow a contact via the incisal pin. They bear plaster keys to fix dental casts (Fig. 2a).
The upper part represents the middle part of the face, especially the Axis-Orbital Plane (AOP). It bears condylar guides representing the mandibular (glenoid) fossae of the temporal bones. Anatomically, they are cavities on the outer surface of these bones, where the mandibular condyles are articulated, thus forming the TMJ. By programming, that is to say by adjusting the condylar guides settings, it is aimed to closer reproduce the anatomy of the mandibular fossae, and get an idea of the condylar kinematic of the patient.
A condylar guide bears a protrusion screw and an anterior stop including a spring. This one allows sticking the condylar bowls (representing the mandibular condyle) to the bottom of their box (Fig. 2b). NWLM is then reproducible. The Bennett angle can be replicated by inserting straight Bennett inserts (angle equal to 0°, 10°, 15° or 20°) and the immediate lateral movement can be replicated by inserting curved Bennett inserts (displacement equal to 0.5 mm, 1 mm or 1.5mm) (Fig. 2c).
The condylar slope can also be programmed on the lateral part of the condylar guides by a setting wheel adjusting the inclination from 0 to 70° by an increment of 5° (Fig. 2a).
The lower (double) part corresponds to the mandible. The condylar bowls on the vertical part, corresponding to the mandibular condyles, articulate with the condylar guides on the upper part. The horizontal part bears the plaster key and an incisal table (on which the incisal pin is placed) steerable so representative of the incisal guidance angle (angulation of the maxillary central incisors’ inner part).
On such an articulator, the upper part is movable and the lower one is fixed, (Fig. 2d) contrary to the anatomical reality, where the mandible is movable. Depending on the manufacturer, the setting modes of determinants are different, by changing the Bennett inserts as above noticed (for instance the articulator Quick Master®, Fag) or by tilting the condylar guides sides (for instance the articulators Perfect ®, Fag or Mark II ®, Denar).
Determinants are required to programme an articulator. These data are issued from a recording system drawing the displacements of the mandibular condyles: the axiograph (Fig. 3a-c). The condylar slope and the Bennett angle or the immediate lateral displacement are so identified, allowing replicating the NWLM. Nevertheless two major disadvantages have to be underlined.
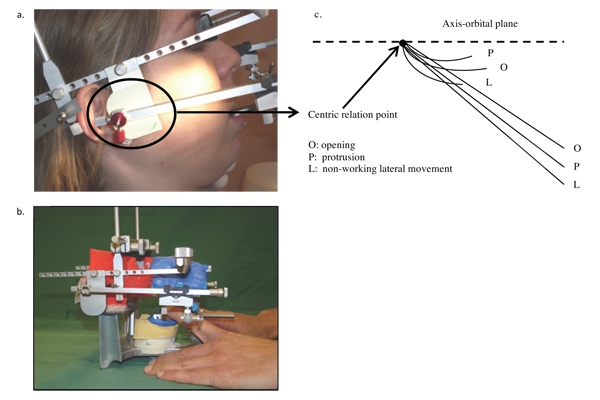 |
Fig. (3). Axiograph (Fag, France): a. on a patient, b. on a semi-physiological articulator, c. standard results. |
On the one hand, the axiography is a non-invasive but time consuming act. It requires a substantial patient involvement, which can lead to uncertain results in case of a non-optimal understanding.
On the other hand, despite the accuracy of the axiographic data, the Bennett inserts only allow to approximate the physiology, as different angulations can match with one insert. Various mandibular movements are not accurately reproduced and they are just an approximation of the real trajectory. This brings up questions about the accuracy of teeth contacts on dental mouldings placed on the articulator (Fig. 2d).
The standard articulator used in our study is the Quick Master ® by Fag company (and its corresponding axiograph). Indeed, it is commonly used within French dental offices because of its programming level and its ease of implementation. Consequently, we use it as a basis for the modified articulator and as a comparative model.
2.2. Modification of a Standard Articulator: CT Scan and Rapid Prototyping
The replacement of the condylar bowls, the Bennett inserts and other devices of adjustment aims to get rid of both the metrology on the patient and the approximation due to the technology of the articulator. It aims to obtain a physiological articulator by adapting on the device a replica of the patient’s condylar guides processed through an additive manufacturing technique from medical imaging data. Therefore, a CT scan replaces the axiography and a rapid prototyped replica of the TMJ replaces the machined condylar guides and bowls.
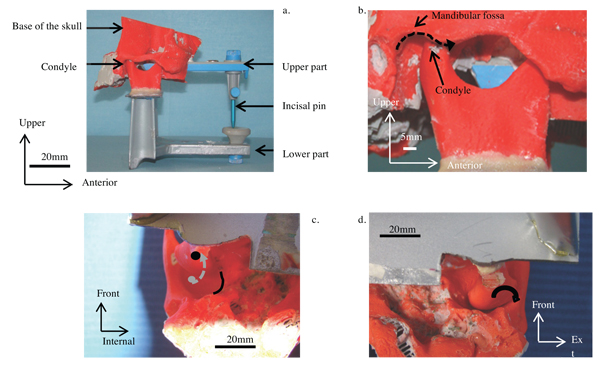
The CT scan [10] aims to anatomically define the base of the skull and the mandible (head in hyperextension and maximal intercuspidation, that is to say in dental occlusion). The obtained slices are 0.6mm thick (247 slices on the average). As the lower jaw is connected to the base of the skull by the TMJ, density filters contribute to the elimination of the dental arches and the surrounding tissues of this joint. The same process leads to isolate the very TMJ, although it is more difficult because the ligament capsule and the cartilaginous articular disc have densities closed to the one of the bone. Moreover, numerous muscle attachments encompass it. The DICOM3 digital files are modified and converted to the STL format through a dedicated software package (Mimics ®, Materialise, Belgium).
The fused deposition modelling (FDM) [11] is chosen to manufacture the anatomical part. This rapid prototyping technique is current, reliable, relatively cheap and able to process complex shaped parts. The machine (Dimension® BST 768, Stratasys, USA) operates a fused deposition of ABS resin filament (acrylonitrile butadiene styrene, 256 µm diameter). The piloting software (Catalyst ®, Stratasys, USA) ensures the 3D file slicing (STL version) in 0.256 mm thick sections.
In order to position the replica, the standard articulator is modified. The modification must enable to simply replace the TMJ elements of the machined articulator by the prototyped parts. There is no modification of the position, only the feasibility is studied. The condylar bowls are cut from the lower part, in order to position the physiological condyles at the same height than the condylar bowls. It aims to precisely substitute the prototyped condyles to the machined ones. The height is calculated so the centre of the condyle accurately corresponds to the centre of the replaced machined condylar bowl. The standard condylar guides are removed from the upper part. The part allowing the condylar guides coherence is cut.
The prototyped part is modified to adjust the articulator. The condyles are cut to ensure the exact substitution of the condylar bowls. Both condyles are first joined to keep the distance between them to ensure their placement in the mandibular fossae.
The base of the skull must be centred to the frontal and sagittal planes in order to join the upper part; it must match the AOP. This plane is chosen because it is easily identifiable both on the medical imaging, the prototyped base and the reference for the orientation of the upper part on several standard articulators. A parallelepiped hole centred to the anterior nasal spine is generated in the base of the skull. A virtual axis passing through the centre of the mandibular fossae defines the depth and its height that matches the AOP.
A 2 mm thick polymethyl methacrylate plate is positioned on the cut lower part. The joined condyles are glued on it, ensuring a perfect horizontal position, placed in the middle of the frontal and sagittal planes.
The upper part is then positioned thanks to a fast set plaster (Snow White®, Kerr). It is placed in the centre of the frontal plane relative to the anterior nasal spine and the sagittal plane relative to the AOP. This latter is located on the prototyped base of the skull thanks to the anatomical elements visible on this latter: the hinge axis and the infraorbital foramen.
The horizontal part is positioned, oriented as on the previously defined plans.
The second generation semi-adjustable articulator is now a semi-physiological articulator.
3. RESULTS AND DISCUSSION
The first advantage of the Semi-Physiological Articulator (SPA) lies in the accurate reproduction of the mandibular kinematic of the patient. Three movements (protrusion, NWLM and WLM) are studied and compared through their replica on the Standard Articulator (SA) and on the SPA (Fig. 4a). Also, the interest consists in replacing the axiography, as the SPA is equipped with an axiograph. The study of axiographic recordings of the condylar slope and the NWLM and the opening movement is performed and the values are compared with those measured on the recordings on the very patient. The aim is to quantify the reproducibility.
3.1. Reproduction of Protrusion, NWLM and WLM on a Standard Articulator and on a Semi-Physiological One
On the Standard Articulator (SA), in the rest position, the condyle bowl lies against the posterior wall of the condylar guide. During the protrusion, the condylar bowl slides along the ceiling of the condyle guide, along a fully straight linear trajectory; only its angulation is adjustable (Fig. 2a).
On the Semi-Physiological Articulator (SPA), in the rest position, the condyle is located on the highest part of the mandibular fossa. During the protrusion, the condyle naturally follows the shape of the ceiling of the fossa. So the trajectory is curved (Fig. 4b). So there is no more choice of the condylar slope angulation to make.
It is clear that the protrusion trajectory on the SA is only a straight linear representation of the real physiological trajectory (Fig. 5).
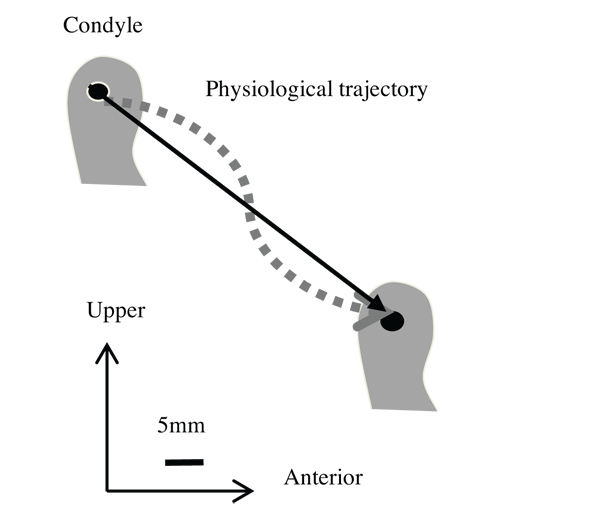 |
Fig. (5). Representation of the condylar trajectory during protrusion on the standard articulator and on the semi-physiological articulator. |
The movement of the non-working condyle (NWLM) is studied in the horizontal plane in order to decompose its trajectory. In rest position the condylar bowl is urged, backward, against the posterior wall of the condylar guide and, inside, against the insert. During the movement, the condylar bowl slides along the shape of the insert, the angle being imposed by this one. Thus, to simulate the NWLM relative to the Bennett angle, a straight insert is positioned (Fig. 2c). Finally, to simulate an immediate lateral movement, a curved insert is positioned.
On the SPA, the condylar trajectory is directly related to the anatomy of the internal wall of the mandibular fossa. So, the choice of inserts becomes unnecessary because the condyle naturally slides along this wall (Fig. 4c), from the back to the front and from the outside to the inside, respecting the anatomy of the mandibular fossa.
The working lateral movement is also studied in the horizontal plane. In rest position, the condylar bowl is in the same position as during the NWLM, that is to say backward on the posterior wall of the condylar guide and inside on the insert. During the lateral movement, the condyle makes a transverse displacement of a few millimetres.
On the SPA the condyle makes a slight twisting movement (Fig. 4d).
The study of the reproduction of the movements on the SPA highlights two important points. On the one hand the quality of the movements realised with the replica of the anatomical elements is logically in accordance with the physiology of the patient. The trajectories, which are directly linked to it, are improved and they look like the real ones. On the other hand, the axiography is no more needed because the prototyped anatomical elements positioned on the articulator do not require determinants to be positioned. Nor do they require programming. So the first source of error, axiography, and the second one, programming, disappear.
3.2. Study Through Axiography of the Semi-Physiological Articulator
The reproducibility of the mandibular movements on the SPA is studied through the axiography. This study enables the representation of the trajectories on which it is possible to measure the angle of the protrusion, of the opening movement and of the NWLM relative to the AOP [12]. Two axiographies are carried out: on the patient and on the articulator (Figs. 3a-b).
The results are graphically collected in situ and they are then transferred on a graph paper to facilitate the measures (Fig. 3c). In order to calculate the angulation of the different trajectories relative to the AOP, their secants are drawn. The starting point of the three trajectories is the same and it corresponds to the centric relation point. However, the trajectories do not have the same length; it leads to define a point 10 mm from the starting point, which is used to draw the secants. The angulation of each secant is measured and the value reported in a Table 1 as for the axiographies on the SPA and on the patient, for the right and left sides.
| Source (side) → Determinant ↓ |
Patient (Right) |
Articulator (Right) |
Patient (Left) |
Articulator (Left) |
|---|---|---|---|---|
| Protrusion | 36° | 32° | 45° | 37.5° |
| Opening | 34° | 27° | 40° | 35° |
| Non-working lateral movt | 39.5° | 36.5° | 46.5° | 42° |
The axiographic plots on the articulator show no aberration relative to the trajectories drawn from the patient. Indeed, when comparing the axiographies the first step consists in a global study of the shape and of the angle of each one. It allows us to check the plottings match before a comprehensive study. In this study the shapes and the orientations are similar. Only the opening movement is less important. This is explained by the fact that there is no elevator muscle on the articulator. By comparing the angulation plots relative to the AOP we can notice that those corresponding to the articulator are less important. This can be explained by the absence of articular discs on the SPA. Indeed, the condyle being highest in the mandibular fossa, in direct bone contact, the angle relative to the AOP is naturally lower. Moreover, the difference between these two types of axiography is generally homothetic, with a loss ranging from 3° to 7.5°, meaning no outlier. It is important to notice that this angulation difference is found both on the left and right recordings. The axiographies show that the reproducibility of the mandibular movements on the SPA is satisfactory. The homothetic decrease of the values is understandable. In fact, this homothety allows validating our results. An aberrant difference between the two sides of the articulator would have been significant of a problem of registration, reproduction or designing of the SPA. The absence of the articular discs cannot be considered as a new gap, since the current standard articulators do not reproduce it either, especially when used without previous programming. The angulation difference will not influence the movements made by our dental casts positioned on the SPA. Thus our aim, which was to overcome the programming of the articulator, can be considered as achieved.
CONCLUSION
The comparison of the different mandibular movements on a new designed and manufactured semi-physiological articulator and on the standard second generation semi-adjustable articulator showed that the reproduction of the mandibular kinematic on the latter is only an approximation of the condylar trajectory in the mandibular fossa, despite its possibility of programming as a function of the patient.
The replica of the TMJ via medical imaging and rapid prototyping and its substitution to the condylar guides may resolve this crucial problem. Indeed, the trajectories depend directly on the anatomy of the joints. Programming the articulator, even accurately, allows only approaching the physiology. For a semi-physiological articulator the very replica of these joints allows us to obtain similar movements to those of the patient. So programming such an articulator is no more required. However, it is not still a physiological articulator because neither muscular and ligament insertions nor the articular discs are reproduced.
Simplifying the protocol strengthens the major advantage of the reproduction of the mandibular movements. Unlike the metrology by axiography, medical imaging, CT scan for instance, is quicker (a few minutes) and processing its data is easier (10 min to differentiate the TMJ). Determining precisely the parts to be prototyped allows to minimize the rapid fabrication step (a few tens of minutes). Finally, the steps require 60 min to obtain a operational articulator but only a few minutes on the patient when the axiography requires an hour of immobilization and when analyzing it and programming the articulator demand much more time.
Furthermore, the X-ray technologies have a very obtainable access and they are increasingly present within dental offices via the cone beam technique for instance. The rapid prototyping technologies, the additive manufacturing techniques for instance, are now also very current. The achievement of a semi-physiological articulator is now within the reach of any dentist. Its simplicity of manufacturing, its easy usability and its clinical interest can make it a successor of standard articulators.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.